Bicuspid aortic valve
Bicuspid aortic valve (BAV) is an inherited form of heart disease in which two of the leaflets of the aortic valve fuse during development in the womb resulting in a two-leaflet valve (bicuspid valve) instead of the normal three-leaflet valve (tricuspid). BAV is the most common cause of heart disease present at birth and affects approximately 1.3% of adults.[2] Normally, the mitral valve is the only bicuspid valve and this is situated between the heart's left atrium and left ventricle. Heart valves play a crucial role in ensuring the unidirectional flow of blood from the atrium to the ventricles, or from the ventricle to the aorta or pulmonary trunk.
| Bicuspid aortic valve | |
|---|---|
| Other names | Bicommissural aortic valve[1] |
 | |
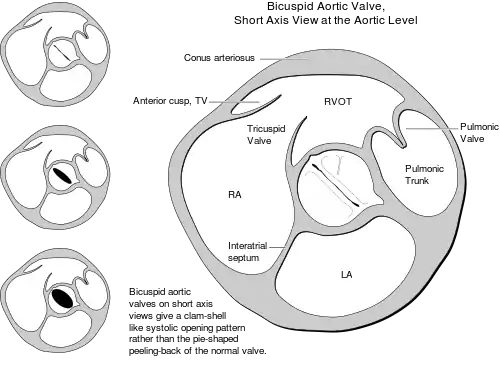
| The aortic valve controls outflow of blood from the left ventricle of the heart through the aorta (valve is indicated within the yellow highlighted box). A normal aortic valve is tricuspid. Five types of bicuspid valve are shown, with Type 1 being most prevalent. A bicuspid valve forms when the tissue surrounding one of the cusps (leaflets) of the valve fuses during fetal development. This developmental anomaly can have either a negative or no effect on the individual. | |
| Specialty | Cardiology |
Signs and symptoms
In many cases, a bicuspid aortic valve will cause no problems.[3] People with BAV may become tired more easily than those with normal valvular function and have difficulty maintaining stamina for cardio-intensive activities due to poor heart performance.
Complications
Calcification
BAV may become calcified later in life, which may lead to varying degrees of severity of aortic stenosis that will manifest as murmurs.[4] If the leaflets do not close correctly, aortic regurgitation can occur.[4] If these become severe enough, they may require heart surgery. The heart is put under more stress in order to either pump more blood through a stenotic valve or attempt to circulate regurgitation blood through a leaking valve.
Aortic lesions
One of the most notable associations with BAV is the tendency for these patients to present with ascending aortic aneurysmal lesions. The extracellular matrix of the aorta in patients with BAV shows marked deviations from that of the normal tricuspid aortic valve. It is currently believed that an increase in the ratio of MMP2 (Matrix Metalloproteinases 2) to TIMP1 (tissue inhibitors of metalloproteinase) may be responsible for the abnormal degradation of the valve matrix and therefore lead to aortic dissection and aneurysm. However, other studies have also shown MMP9 involvement with no differences in TIMP expression. The size of the proximal aorta should be evaluated carefully during the workup. The initial diameter of the aorta should be noted and annual evaluation with CT scan, or MRI to avoid ionizing radiation, should be recommended to the patient; the examination should be conducted more frequently if a change in aortic diameter is seen. From this monitoring, the type of surgery that should be offered to the patient can be determined based on the change in size of the aorta.
Aortic narrowing
A bicuspid aortic valve may cause the heart's aortic valve to narrow (aortic stenosis).[4] This narrowing prevents the valve from opening fully, which reduces or blocks blood flow from the heart to the body. In some cases, the aortic valve does not close tightly, causing blood to leak backward into the left ventricle.[5]
Coarctation of the aorta (a congenital narrowing in the region of the ductus arteriosus) has also been associated with BAV.[6]
Pathophysiology
Fusion of aortic valve leaflets occurs most commonly (≈80%) between the right coronary and left coronary leaflets (RL), which are the anterior leaflets of the aortic valve.[7][8] Fusion also occurs between the right coronary and noncoronary leaflets (RN, ≈17%), and least commonly between the noncoronary and left coronary leaflets (≈2%).[7][8] In comparison to other fusion patterns, RN leaflet fusion has a stronger association with future complications such as aortic valve regurgitation and stenosis.[9][10] However, all fusion patterns associate with a specific area or areas of dilated enlargement in either the root of the ascending aorta, the ascending aorta, or the transverse aortic arch.[7][8][9][11]
Hemodynamics
Identifying hemodynamic patterns in the aorta after left ventricle systole aids in predicting consequential complications of bicuspid aortic valve.[7][8][9] The patient-specific risk of developing complications such as aortic aneurysms is dependent on the particular aortic leaflet fusion pattern, with each pattern varying in 4D MRI measurements of wall shear stress (WSS), blood flow velocity, asymmetrical flow displacement and flow angle of the aorta.[7][8][11]
BAV outflow is helical and occurs at high velocities (>1 m/s) throughout the ascending aorta.[7][8][9] This is potentially more damaging to the aorta in comparison to the streamline flow and short-lived burst of high velocity at the beginning of the aorta, as seen within a healthy tricuspid valve.[7] This eccentric outflow from the BAV results in blood hitting and reflecting off the aortic wall in a non-streamline fashion.[7][8] The specific zones where blood hits is dependent on the varying BAV leaflet fusion patterns and consequently correlates with increases in WSS.[7][11] WSS measurements in RL fusion indicate an increase in pressure applied predominantly to the right-anterior side of the vessel wall, while RN fusion increases WSS on the right-posterior wall.[7][11] The resulting rise in WSS is supported by the asymmetrical displacement of blood flow produced by an increased angle of outflow from the BAV.[7][8] Displacement is measured as the distance in millimeters from the center of the aorta to the center of the high velocity outflow.[7] Blood does not flow centrally through the aorta in BAV, but along the right-anterior and right-posterior vessel wall for RL and RN leaflet fusion respectively.[7][8]
Aortic disease
Identification of hemodynamics for RL, RN, and left coronary and noncoronary leaflet fusion patterns enables detection of specific aortic regions susceptible to dysfunction and the eventual development of disease.[7][8] Specifically, RL and RN fusion patterns are more likely to develop into these aortic disease states.[7][8] The blood flow information associated with RL fusion causes dilation of the mid-ascending aorta, while RN fusion is associated with dilation in the root, distal ascending aorta and transverse arch.[7][9] BAV helical and high velocity outflow patterns are consistent with aortic dilation hemodynamics seen in those with tricuspid aortic valves.[12] However, it is the increase and variance in WSS and flow displacement in BAV that demonstrate the importance of aortic leaflet morphology.[7] Flow displacement measurements taken from 4D MRI may be best for detecting irregularities in hemodynamics.[7] Displacement measurements were highly sensitive and distinguishable between different valve morphologies.[7] Hemodynamic measurements from 4D MRI in patients with BAV are advantageous in determining the timing and location of repair surgery to the aorta in aortopathy states.[7]
Most patients with bicuspid aortic valve whose valve becomes dysfunctional will need careful follow-up and potentially valve replacement at some point in life. Regular EchoCG and MRI may be performed.
If the valve is normally functioning or minimally dysfunctional, average lifespan is similar to that of those without the anomaly.[13]
Diagnosis

A bicuspid aortic valve can be associated with a heart murmur located at the right second intercostal space. Often there will be differences in blood pressures between upper and lower extremities. The diagnosis can be assisted with echocardiography or magnetic resonance imaging (MRI). Four-dimensional magnetic resonance imaging (4D MRI) is a technique that defines blood flow characteristics and patterns throughout the vessels, across valves, and in compartments of the heart.[7][8][14] Four-dimensional imaging enables accurate visualizations of blood flow patterns in a three-dimensional (3D) spatial volume, as well as in a fourth temporal dimension.[7][9][12][14] Current 4D MRI systems produces high-resolution images of blood flow in just a single scan session.[7][14]
Classification
Bicuspid aortic valves may assume three different types of configuration:[15]
- "Real" bicuspid valves with two symmetric leaflets
- A tricuspid architecture with a fusion of two leaflets
- A tricuspid architecture with a fusion of three leaflets
Treatment
Complications stemming from structural heart issues are most often treated through surgical intervention, which could include aortic valve replacement, or balloon valvuloplasty.[16]
Prognosis
BAV frequently leads to significant complications in over one-third of affected individuals which often lead to significant morbidity and mortality.[17] Notable complications of BAV include narrowing of the aortic valve opening, backward blood flow at the aortic valve, dilation of the ascending aorta, and infection of the heart valve.[17]
If aortic regurgitation and dilation of the ascending aorta are noted in someone, they should undergo yearly surveillance with transthoracic echocardiograms if the aortic root measures 4.5 centimeters or greater in diameter.
Epidemiology
Bicuspid aortic valves are the most common cardiac valvular anomaly, occurring in 1–2% of the general population. It is twice as common in males as in females.[18]
Bicuspid aortic valve is a heritable condition, with a demonstrated association with mutations in the NOTCH1 gene.[19] Its heritability () is as high as 89%.[20] Both familial clustering and isolated valve defects have been documented. Recent studies suggest that BAV is an autosomal dominant condition with incomplete penetrance. Other congenital heart defects are associated with bicuspid aortic valve at various frequencies, including coarctation of the aorta.[21]
Bicuspid aortic valve abnormality is also the most observed cardiac defect in Turner syndrome.
References
- "Bicuspid aortic valve : MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 27 May 2019.
- Verma, S; Siu, SC (May 2014). "Aortic dilatation in patients with bicuspid aortic valve". New England Journal of Medicine (Review). 370 (20): 1920–9. doi:10.1056/NEJMra1207059. PMID 24827036. S2CID 55778596.
- "Atrial Septal Defect". Commonly Asked Questions About Children and Heart Disease. October 29, 2012. Retrieved April 9, 2014.
- Ward, C. (2000-01-01). "Clinical significance of the bicuspid aortic valve". Heart. 83 (1): 81–85. doi:10.1136/heart.83.1.81. ISSN 1355-6037. PMID 10618341.
- Aortic valve stenosis (AVS). American Heart Association. http://www.heart.org/HEARTORG/Conditions/CongenitalHeartDefects/AboutCongenitalHeartDefects/Aortic-Valve-Stenosis-AVS_UCM_307020_Article.jsp#.WclzKdjrvcs. Accessed December 23, 2018.
- Rison, S. C. G.; Locke, T. P.; Rosenthal, E.; Gandhi, S. (2012). "A man with hypertension and two murmurs". BMJ. 344 (feb15 1): e956. doi:10.1136/bmj.e956.
- Mahadevia R, Barker AJ, Schnell S, et al. (February 2014). "Bicuspid aortic cusp fusion morphology alters aortic three-dimensional outflow patterns, wall shear stress, and expression of aortopathy". Circulation. 129 (6): 673–82. doi:10.1161/CIRCULATIONAHA.113.003026. PMC 3946057. PMID 24345403.
- Bissell MM, Hess AT, Biasiolli L, et al. (July 2013). "Aortic dilation in bicuspid aortic valve disease: flow pattern is a major contributor and differs with valve fusion type". Circulation: Cardiovascular Imaging. 6 (4): 499–507. doi:10.1161/CIRCIMAGING.113.000528. PMC 3859916. PMID 23771987.
- Hope MD, Hope TA, Meadows AK, et al. (April 2010). "Bicuspid aortic valve: four-dimensional MR evaluation of ascending aortic systolic flow patterns". Radiology. 255 (1): 53–61. doi:10.1148/radiol.09091437. PMID 20308444.
- Fernandes SM, Sanders SP, Khairy P, et al. (October 2004). "Morphology of bicuspid aortic valve in children and adolescents". Journal of the American College of Cardiology. 44 (8): 1648–51. doi:10.1016/j.jacc.2004.05.063. PMID 15489098.
- Barker AJ, Lanning C, Shandas R (March 2010). "Quantification of hemodynamic wall shear stress in patients with bicuspid aortic valve using phase-contrast MRI". Annals of Biomedical Engineering. 38 (3): 788–800. doi:10.1007/s10439-009-9854-3. PMC 2872988. PMID 19953319.
- Weigang E, Kari FA, Beyersdorf F, et al. (July 2008). "Flow-sensitive four-dimensional magnetic resonance imaging: flow patterns in ascending aortic aneurysms". European Journal of Cardio-Thoracic Surgery. 34 (1): 11–6. doi:10.1016/j.ejcts.2008.03.047. PMID 18515137.
- Michelena HI, Desjardins VA, Avierinos JF, et al. (May 2008). "Natural history of asymptomatic patients with normally functioning or minimally dysfunctional bicuspid aortic valve in the community". Circulation. 117 (21): 2776–84. doi:10.1161/CIRCULATIONAHA.107.740878. PMC 2878133. PMID 18506017.
- Markl M, Chan FP, Alley MT, et al. (April 2003). "Time-resolved three-dimensional phase-contrast MRI". Journal of Magnetic Resonance Imaging. 17 (4): 499–506. doi:10.1002/jmri.10272. PMID 12655592.
- Kumme, Anja (2007). Klassifikation bikuspider Aortenklappen. OCLC 254078723.
- Mohler ER, et al. Management of thoracic aortic aneurysm in adults. https://www.uptodate.com/contents/search. Accessed December 23rd, 2018.
- LaHaye, S; Lincoln, J; Garg, V (2014). "Genetics of valvular heart disease". Current Cardiology Reports (Review). 16 (6): 487. doi:10.1007/s11886-014-0487-2. PMC 4531840. PMID 24743897.
- Tzemos N, Therrien J, Yip J, et al. (September 2008). "Outcomes in adults with bicuspid aortic valves". JAMA. 300 (11): 1317–25. doi:10.1001/jama.300.11.1317. PMID 18799444.
- Garg V, Muth AN, Ransom JF, et al. (2005). "Mutations in NOTCH1 cause aortic valve disease". Nature. 437 (7056): 270–274. Bibcode:2005Natur.437..270G. doi:10.1038/nature03940. PMID 16025100.
- Cripe L, Andelfinger G, Martin LJ, Shooner K, Benson DW (July 2004). "Bicuspid aortic valve is heritable". Journal of the American College of Cardiology. 44 (1): 138–43. doi:10.1016/j.jacc.2004.03.050. PMID 15234422.
- Blackbourne, Lorne H.; Chhabra, Anikar, eds. (2002). "Congenital Heart Disease". Pathology Recall. Lippincott Williams & Wilkins. pp. 247–9. ISBN 978-0-7817-3406-6.
| Classification | |
|---|---|
| External resources |